Introduction
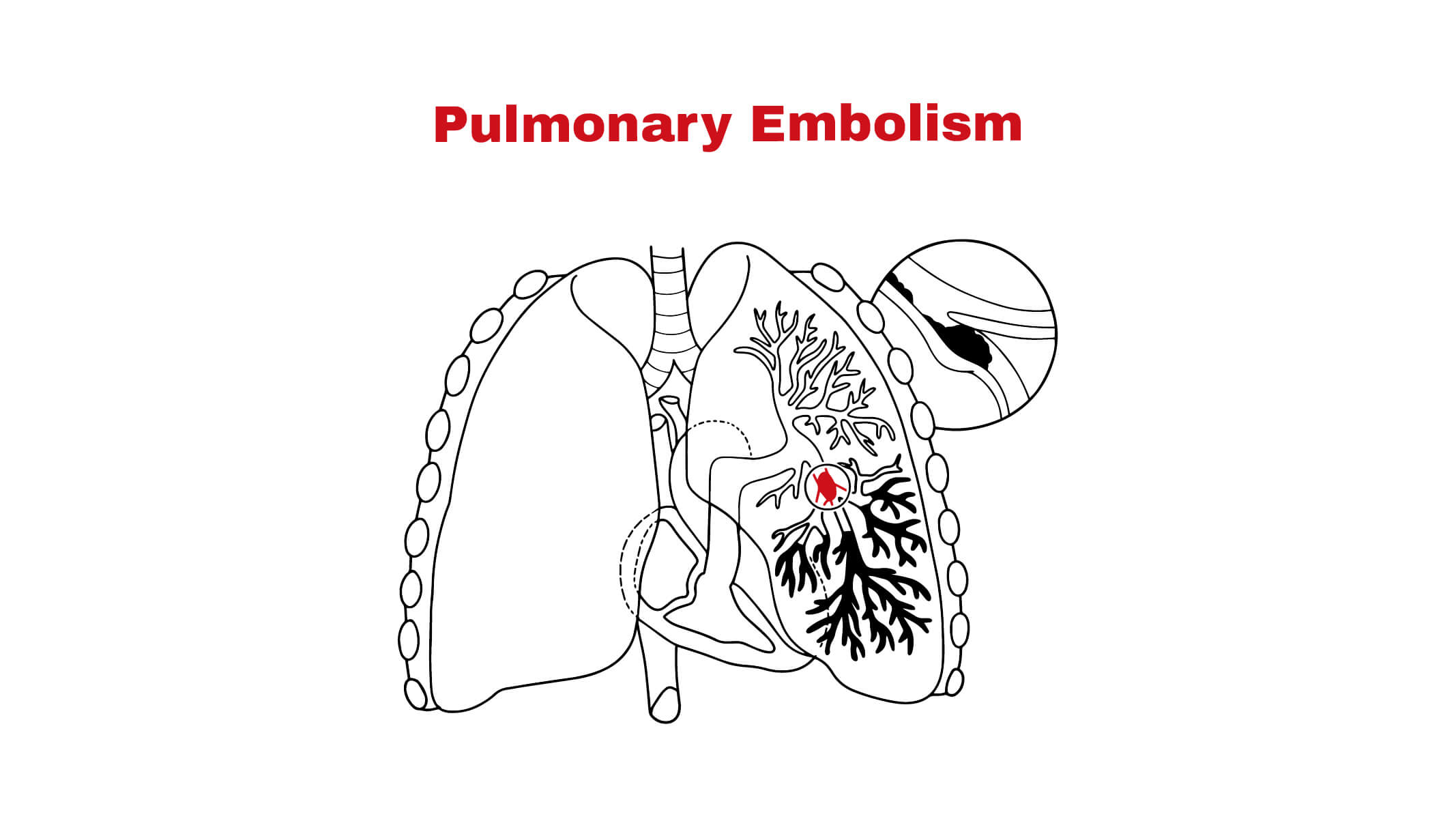
Pulmonary embolism is an obstruction of blood clots in pulmonary arteries that supply blood into the lungs. It occurs due to the blocked arteries in the lungs. When a pulmonary artery is blocked, blood cannot flow appropriately between the heart and lungs. The slow blood flow can lead to clotting. Blood clotting mostly comes from the deep veins of the legs and travels from the heart to the lungs. The clots of blood flow in the lungs can be life-threatening.
Causes of pulmonary Embolism:
There are different causes of this disease, which may include:
- Blood clot: PE is caused by a blood clot. The blood clot mainly comes from the legs’ deep veins, especially the pelvis or thigh. This type of blood clotting is often referred to as deep vein thrombosis.
- Prolonged immobility: When blood clots form, the blood flow slows down in the legs. Mostly happens when a person is on bed rest or in hospital for a long time. Moreover, it also occurs after a long drive or flight and in paralysis.
- Injury or surgery: Injury or orthopedic surgery (especially in the knee, legs, or pelvis) can cause a pulmonary embolism.
- Cardiovascular diseases: Such as atrial fibrillation, heart attack, high blood pressure, congestive heart failure, and stroke may cause a pulmonary embolism.
- Family history: Pulmonary Embolism can occur if a person has a family history of blood clotting and other clotting disorders.
- Medications: It can be caused by certain medications, such as estrogen therapies and birth control pills.
- Older adults: This life-threatening disease is common in older adults.
- After childbirth: Pulmonary Embolism can rarely occur during or after birth.
- Other substances: Pulmonary Embolism can cause by fat droplets, air bubbles, or amniotic fluids, but it is less common.
Symptoms:
Pulmonary embolism has different symptoms depending upon the severity of blood clots. These symptoms are as follows:
- Chest pain
- Breathing difficulty
- Coughing with blood
- Fever
- Excessive sweating
- Swelling and pain in the legs
- Rapid heartbeat
- Wheezing
- Discoloration of skin
- Lightheadedness
- Heart palpitations (fluttering or rapid heartbeat)
- Anxiety
- Hypoxemia
- Fainting or dizziness
- Redness and tenderness in the legs
Chest pain: It is primarily a burning sensation that feels like a heart attack. People often felt worse chest pain while taking deep breaths, and this sharp pain stopped them from taking breaths. In addition, people may also feel chest pain when they bend or cough.
Difficulty breathing: It is the most common symptom of pulmonary embolism and starts suddenly during exerting and sleeping.
Diagnosis:
When you feel chest pain, breathing difficulties, and cough with bloody mucus, visit the doctor immediately. The specialist suggests specific tests to detect pulmonary embolism, which may include:
- Chest X-rays: An imaging test that uses X-rays to evaluate the organs and structures of the heart and lungs. It estimates the shape, size, and location of the bronchi, lungs, heart, pulmonary arteries, and aorta.
- Pulmonary angiogram: It is used to see a detailed image of the blood vessels in the lungs. A pulmonary angiogram evaluate certain conditions, for example, stenosis, aneurysm (bulge in the blood vessel), and blockages. In this procedure, the dye is inserted using a thin tube placed in the pulmonary arteries.
- CT scan: CT scan uses X-rays to create detailed images of the lungs, heart, and muscles and to detect abnormalities. It shows the picture of blood vessels within the lungs.
- Duplex ultrasound uses sound waves to create pictures of the tissues, organs, and blood vessels. Furthermore, it evaluates the structure within the blood vessels and blood flow.
- Ventilation-perfusion scan: In this test, a radioactive substance is used to detect pulmonary embolism. A ventilation scan assesses the ventilation into or out of the bronchioles. The perfusion scan is used to check the blood flow in the lungs.
- Chest MRI: In this test, radio waves and a magnetic field are used to create detailed images of the structures in the chest area.
- Electrocardiogram: It is used to check electrical activity and heart rhythm. Electrodes are attached to the chest at different spots to examine the heart problems.
- Blood tests, such as D dimer, examine the presence of blood clots.
Treatment:
The treatment depends on the patient’s medical history and disease symptoms. A doctor recommends medications and a healthy lifestyle to treat the signs and symptoms. Furthermore, the doctor suggests a nutritious diet, avoiding tobacco, daily exercise, or physical activity to maintain a healthy lifestyle. It may require specific medications, such as:
- Anticoagulants: These medications are blood thinners used to reduce blood clotting. It also decreases the formation of new clots. There are certain anticoagulant medications, such as heparin, warfarin, Lovenox, and fondaparinux. Furthermore, heparin is used as liquid medication, and fondaparinux injects subcutaneously. The doctor also suggests anticoagulants if a person has been hospitalized after a heart attack or stock.
- Fibrinolytic therapy: These medications are referred to as clot busters. Fibrinolytic therapy is used to break the clot and prevent life-threatening conditions.
- Pulmonary embolectomy: This procedure is used to remove the pulmonary emboli. When pulmonary emboli are large, pulmonary embolectomy can be done in severe conditions.
- Percutaneous thrombectomy: A thin, long tube (catheter) is inserted into the embolism using X-rays. A catheter is used to break the embolism using thrombolytic therapy.
- Vena cava filter: This filter stops blood clots from the heart to the lungs and prevents pulmonary embolism.
Risk factors:
These are the factors that boost the risk for pulmonary embolism, which may include:
- Covid-19: Covid-19 enhances the risk factors for pulmonary embolism.
- Obesity: Obesity increases the risk factors of pulmonary embolism and deep vein thrombosis equally among men and women.
- Smoking: Cigarette smoking can increase the risk factors of pulmonary embolism by damaging the blood vessels.
- Tumor: The blockage of blood flow in the lungs may be due to cancer cells. About 1% to 2% of cancer deaths are caused by pulmonary embolism. Certain cancers, such as brain, pancreas, ovary, lung, kidney, and stomach, enhance blood clotting risk factors. Furthermore, cancer therapies, including chemotherapy, also enhance the risk.
References:
https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647#
https://www.webmd.com/lung/what-is-a-pulmonary-embolism
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pulmonary-embolism
https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/pulmonary-embolus#